Health Right Here: Understanding Hemodialysis for Kidney Failure
End Stage Renal Disease Vascular Access Options
When kidneys stop cleaning the blood effectively, known as end-stage renal disease (ESRD), vascular access for dialysis becomes essential for patient survival and quality of life. There are several vascular access options available, including central venous catheters, arteriovenous (AV) fistulas, and AV grafts. Each option has its advantages and disadvantages, but AV fistulas are generally considered the gold standard due to their lower infection rates and better long-term outcomes. As shown in the figure, patients receiving fistulas demonstrate improved survival over 5 years.
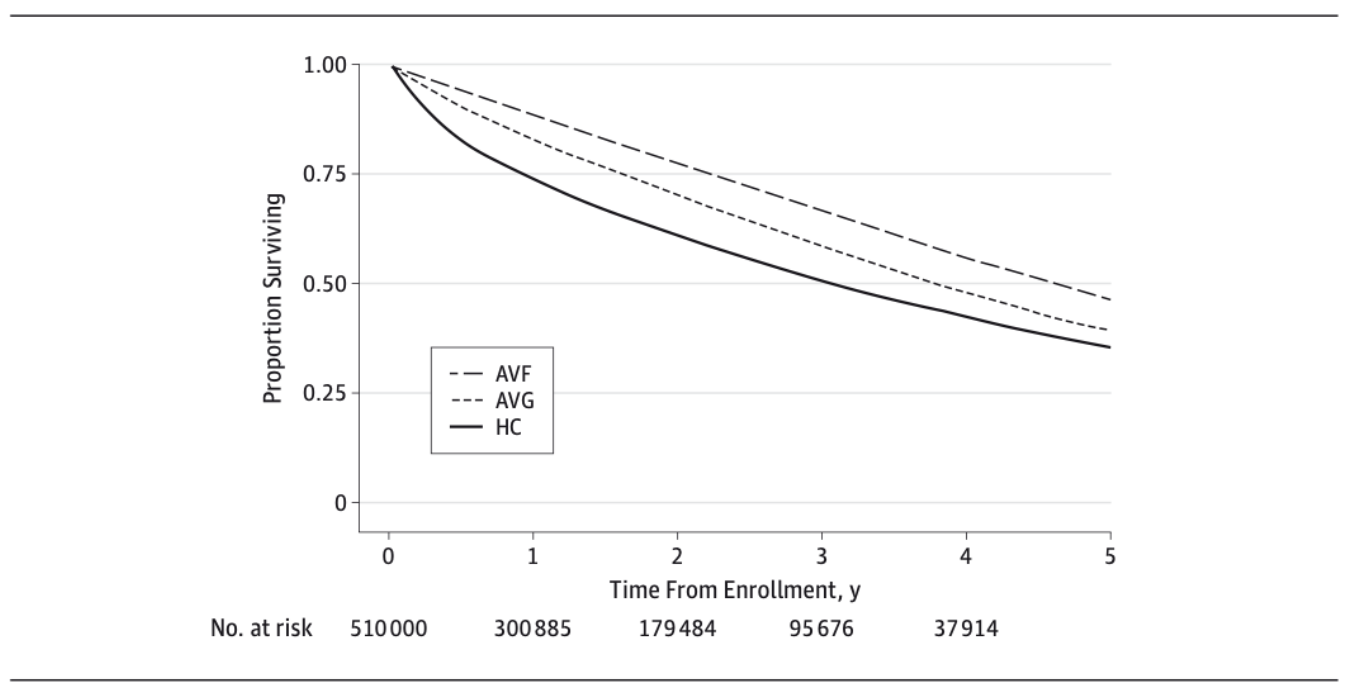
Figure. Patient survival over 5 years based on vascular access type.
Malas MB, Canner JK, Hicks CW, Arhuidese IJ, Zarkowsky DS, Qazi U, Schneider EB, Black JH 3rd, Segev DL, Freischlag JA.JAMA Surg. 2015 May;150(5):441-8. doi: 10.1001/jamasurg.2014.3484.
Single Site Percutaneous Arteriovenous Fistula Creation
A significant advancement in vascular access for dialysis is the technique of single site percutaneous arteriovenous fistula (psAVF) creation, which can be performed in an office setting. This minimally invasive procedure allows for the creation of an AV fistula through a small puncture rather than open surgery, providing patients with the survival advantage of a fistula without requiring a trip to the hospital. Fistula creation involves ultrasound guidance and specialized devices, enabling the surgeon to create a functional AV fistula with reduced recovery time and complications.
One of the main advantages of the psAVF technique is its ability to be performed under local anesthesia, making it accessible for patients who may not be suitable for traditional surgical approaches due to comorbidities. Additionally, this method can significantly reduce hospital visits and associated healthcare costs. Patients often appreciate the convenience and comfort of receiving this procedure in an outpatient setting.
Medicare Part B Qualification for ESRD Patients
For patients with ESRD, Medicare provides coverage under Part B, particularly for dialysis services and related care. To qualify for Medicare Part B, patients must meet specific criteria, including being eligible for Social Security – usually age over 65 years old - or Railroad Retirement benefits or having been diagnosed with ESRD and requiring dialysis or kidney transplantation. This coverage includes necessary outpatient services such as dialysis, laboratory tests, and physician visits.
Medicare Part B vs. Medicare Advantage and IPAs
Medicare Part B offers traditional fee-for-service coverage, allowing patients the flexibility to choose their healthcare providers. Conversely, Medicare Advantage plans, also known as Part C, often include additional benefits but may require patients to use a network of doctors and facilities. These plans may have lower out-of-pocket costs but limit access to certain specialists or treatments.
Integrated Practice Associations (IPAs) are groups of healthcare providers that come together to provide coordinated care for Medicare patients. IPAs often contract with Medicare Advantage plans, offering services under a capitated payment model, which can incentivize preventive care but may also limit treatment options based on contractual agreements.
Conclusion
As the demand for effective vascular access solutions continues to rise, innovations like single site percutaneous arteriovenous fistula creation in the office setting represent significant advancements in patient care. All folks with ESRD on dialysis are eligible for Medicare Part B benefits. Be sure to consider coverage options during the next open enrollment period, starting with www.medicare.gov